Silica dust is among the most under-recognised health hazards at many workplaces where concrete, stone, bricks or engineered materials are processed. It doesn’t scream for attention; it drifts unseen. Over time, however, inhalation of respirable crystalline silica (RCS) causes irreversible lung damage, serious diseases, and even death.
According to HSE, silica is the biggest risk to construction workers after asbestos. The risk is not static: evolving work practices, new materials (like engineered stone), and inadequate controls mean exposure is still common in many UK sites.
In this blog, we will explore:
- What is Respirable Crystalline Silica (RCS)
- Biology of Silica Dust Damage
- Diseases Caused by Silica Dust
- HSE Guidance, Standard & Updated Health Surveillance
- Why Silica Dust Remains a Threat Today
- Health Surveillance Draws the Clear Line of Defence
- Best Practices for Exposure Control
- Putting It All Together
- FAQs
What is Respirable Crystalline Silica (RCS)?
Silica (silicon dioxide) is naturally occurring mineral in many rocks, sand, concrete, clay and masonry. However, many may not realise:
- Not all silica is harmful; it becomes dangerous when processed into respirable particles (RCS) small enough (<10 micrometres) to reach the deep lung.
- These particles are invisible and lightweight; you may inhale them without ever noticing.
When materials that have silica are cut, drilled, ground, polished or crushed, these fine particles are released into the air. The dust matters are the respirable fraction, the microscopic dust that evades the body’s natural defence mechanisms and lodges deep in lung tissue.
HSE’s guidance on stoneworker safety emphasis that exposure depends on type of stone (natural versus engineered), the tools used, duration of work, efficiency of extraction, ventilation, and the effectiveness of RPE (respiratory protective equipment).
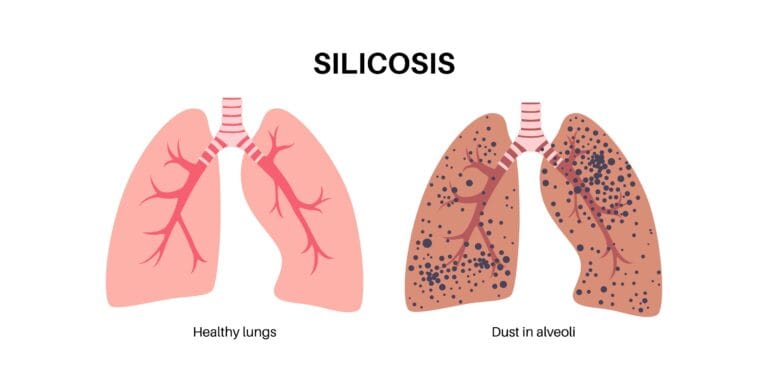
Biology of Silica Dust Damage
The Inflammatory Cascade & Fibrosis
Once inhaled, silica particles are attacked by immune cells (macrophages). These cells attempt to engulf the particles but typically do not digest crystalline silica. Instead, they rupture, realising inflammatory mediators (cytokines) and reactive oxygen species. Over time, repeated injury leads to fibrosis, or scarring, of lung tissue.
This smothering of the alveolar (air exchange) region:
- Reduce lung elasticity.
- Lower gas exchange capacity.
- Increase susceptibility to infections.
Once fibrosis is established, the process is irreversible.
Latency and Silent Progression
One of the cruellest attributes of silica disease is latency. A worker may inhale harmful levels for years before symptoms manifest. By the time breathlessness, cough or chest pain appear, significant damage is often done. This is why proactive surveillance is so essential.
Diseases Caused by Silica Dust
Silica dust exposure is implicated in multiple serious health conditions. Below are key conditions employers and employees should know:
- Silicosis – A chronic, irreversible lung disease characterised by progressive fibrosis. Symptoms include breathlessness, cough, and eventual respiratory failure.
- Acute Silicosis – Occurs after very high short-term exposure; can progress rapidly (months instead of years).
- Chronic Obstructive Pulmonary Disease (COPD) – Silica dust contributes to airway obstruction and chronic respiratory disability.
- Lung Cancer – The International Agency for Research on Cancer (IARC) classifies crystalline silica as a Group 1 carcinogen.
- Other Associations – kidney disease, autoimmune conditions (e.g. rheumatoid arthritis), tuberculosis susceptibility.
HSE also estimates that over 500 construction workers die annually from silica-related diseases.
Another often-cited statistic: at the current UK workplace exposure limit (WEL) of 0.1mg/m3, HSE estimates 30 in every 100 workers exposed over a lifetime may develop silicosis. Reducing exposure to 0.05 mg/m3 would cut this to about 5 in 100.

HSE Guidance, Standards, & Updated Health Surveillance
Workplace Exposure Limit & Legal Framework
Under Control of Substances Hazardous to Health Regulations 2002 (COSHH), employers must control hazardous exposure, monitor levels, and provide health surveillance.
The Workplace Exposure Limit (WEL) for respirable crystalline silica in Great Britian is defined as 0.1 mg/m3 (8-hour time weighted average).
However, the WEL is not a “safe level,” it’s a maximum. HSE emphasises that exposure must be reduced as low as is reasonably practicable (ALARP).
In March 2025, HSE updated the guidance “Health surveillance for those exposed to respirable crystalline silica (G404)”, clarifying employer and occupational health professional responsibilities. The update specifically names worktop manufacturing/installation and stone masonry as high-risk occupations.
Key takeaways from the update:
- Health surveillance must be considered when workers are regularly exposed to RCS and may develop silicosis.
- Surveillance must not replace proper risk assessment and control.
- If a worker shows signs of diseases, risk controls must be reviewed immediately.
- Employers must consult occupational health professionals to tailor surveillance programmes.
Silica Dust Case Studies & Lessons Learnt
There is a stoneworker who developed silicosis after more than 30 years working with stone, including marble and sandstone with high crystalline silica content.
Terry’s case underscores the silent buildup of damage and the lifelong impact of inadequate protection. It represents a human face behind regulatory numbers, a worker whose life has been permanently altered by cumulative exposure.
In 2023, HSE fined Warmsworth Stone Limited for repeated failures to protect employees from RCS exposure. Among other breaches, the company ignored multiple improvement notices, lacked adequate ventilation, and did not monitor exposure. They were fined £18,000 and ordered to pay costs.
This case illustrates the regulatory consequences of neglect and proves the HSE is actively enforcing compliance in high-risk sectors.
Why Silica Dust Remains a Threat Today
Engineered Stone & Emerging Risks
Engineered stone (popular for kitchen worktops) often contains >90% crystalline silica, far more than natural stone.
Globally, clusters of accelerated silicosis (onset in younger workers, rapid progression) have been linked to engineered stone fabrication and installation.
In the UK, early cases have been reported, prompting calls for stricter regulation or bans.
Evolving Tools & Work Practices
Dust production from modern power tools, portable systems, and dry cutting techniques is frequently orders of magnitude more than that from manual techniques, particularly in cases where controls are insufficient or non-existent.
During cutting or grinding, even brief episodes of excessive dust might result in spikes that are significantly higher than the WEL.
Residual & Secondary Exposure
Silica dust doesn’t just vanish. It clings to:
- Clothing
- Surfaces (floors, tables)
- Tools and machinery
Workers can be re-exposed later via re-aerosolisation or carry dust home, endangering themselves and others.
Health Surveillance Draws the Clear Line of Defence
Given the latent nature of silica disease, health surveillance is indispensable. Early detection can mean the difference between manageable impairment and debilitating disease.
What Does Health Surveillance Involve?
- Baseline assessment before exposure begins.
- Chest X-rays (silica-specific protocols) to find scarring patterns.
- Spirometry / lung function testing (FEV1, FVC, etc.)
- Symptom questionnaires (cough, breathlessness, chronic infections)
- Periodic reviews (every 1–3 years or more often if risk is high)
- Medical interpretation by occupational health professionals
If surveillance detects signs of disease or deterioration, controls must be reassessed, and the worker may be reassigned or removed from exposure.
How Early Detection Protects
- Allows prompt intervention before disease advances.
- Triggers upgrade of dust controls or process changes.
- Reduces likelihood of severe disease, compensation claims, and reputational damage.
HSE’s updated guidance emphasises that surveillance results should feed back into risk assessment and control revisions.
Best Practices for Exposure Control
The classic hierarchy of controls still applies. According to HSE, employers should systematically apply:
1. Elimination / Substitution
Avoid using materials with high silica content, or switch to alternative materials when possible.
2. Engineering Controls
- On-tool extraction and dust suppression (water sprays).
- Local exhaust ventilation (LEV) with regular inspection (test every 14 months minimum).
- Enclosed processes or barriers to isolate dust generation.
3. Administrative Controls
- Limit time spent in dusty tasks.
- Job rotation to reduce individual cumulative exposure.
- Cleaning regimes using vacuum (HEPA) or damp methods, never dry sweeping.
- Training, signage, and safe work procedures.
4. Personal Protective Equipment / RPE
Use only when higher-level controls do not fully cut exposure. Fit-testing, filter-change schedules, and strict usage protocols are essential.
5. Review & Monitoring
Periodic air sampling to verify that controls stay effective (personal and area sampling).
It is vital to treat RPE not as a primary defence but as a fallback measure.
Putting It All Together
Consider a stone fabrication facility:
- Workers cut engineered stone on site without water suppression.
- Dust drifts freely, contaminating floors, walls, and clothing.
- No health surveillance or exposure monitoring is in place.
This setup invites disaster.
Now imagine upgraded practices:
- Pre-cut slabs are used, eliminating onsite cutting.
- All cuts are made with on-tool water suppression and extraction.
- Workers rotate tasks to limit cumulative exposure.
- RPE (FFP3 / P3) is used only where controls can’t fully eliminate dust.
- Healthscreen UK provides baseline and periodic silica X-rays & lung testing.
- Results feed back into improvements, e.g. enhanced extraction, better scheduling, or switching to lower-silica mixes.
Such an integrated approach turns a silent threat into a managed risk.
At Healthscreen UK, we provide comprehensive Silica X-rays and lung testing to help businesses stay compliant and safeguard employee health. Our specialists deliver both on-site and clinic-based assessments, complete with clear medical reports and, when needed, referrals to trusted hospitals for further care. To learn more or request a quote, contact Healthscreen UK today, because protecting your team’s lungs means protecting your business.
FAQs
1. How to remove silica dust from lungs?
Once RCS is inhaled, it cannot be removed. The aim is early detection (via X-rays and lung testing) and prevention of further accumulation. Avoiding smoking, maintain good general health, and remove or reduce further exposure can slow disease progression.
2. Is silica as bad as asbestos?
Yes, in many respects. Both are silent inhaled carcinogens causing irreversible lung disease. While asbestos may be more notorious, HSE recognises silica as the second greatest risk to construction workers. The severity lies in continued exposure across thousands of worksites.
3. How often should silica X-rays and lung tests be carried out?
HSE recommends baseline health surveillance, followed by periodic testing every one to three years, depending on exposure risk and job role. More frequent checks may be needed in high-risk tasks or where deterioration is observed.
4. Can you wash silica dust out of your clothes?
Yes, safely. Work clothing should be washed separately, preferably via on-site laundry or a professional facility. Avoid shaking out garments, using home washing machines or dry-cleaning methods, as that can re-release silica dust into the air.
5. How can employers arrange silica X-rays and lung tests?
Employers can engage a competent occupational health provider (e.g. Healthscreen UK) to schedule on-site or clinic-based silica X-rays, spirometry, symptom screening, and reporting, all in compliance with HSE and COSHH obligations.